Lymphedema
On this page, we explain the origin, causes, symptoms and the different stages of lymphedema.
What is Lymphedema?
Lymphedema refers to swelling of the tissue as a result of retained fluid. This swelling occurs when more fluid accumulates in the tissue than can be removed. Possible causes include inflammation (e.g. an insect bite or an injured ankle), which leads to a temporary overload of the lymphatic system – this is called acute lymphedema. Once the inflammation subsides, the tissue swelling also decreases.
On the other hand, the lymphatic system may also be chronically, i.e. permanently, disrupted. In this case, it is advisable to start appropriate treatment as soon as possible to prevent the condition from deteriorating.
Depending on whether lymphedema is hereditary or develops later in life, we differentiate between "primary" and "secondary" lymphedema.

Congenital: Primary Lymphedema
In people with primary lymphedema, the defective structure of the vascular system is congenital. However, the deformation is only rarely visible after birth, as the functioning vessels can still compensate for the defect. Lymphedema only becomes noticeable as swellings when the healthy vessels can no longer withstand the additional strain, for example during puberty or due to injuries.
The following deformations can lead to disorders of the lymphatic system:
- Individual lymph vessels or lymph nodes are missing.
- The number of lymph vessels is too small.
- Lymph vessels are constricted or dilated.
- Lymph vessels are hardened.

Damaged: Secondary Lymphedema
Secondary lymphedema occurs more frequently than primary lymphedema. It is characterized by the fact that the lymphatic system has been damaged through external influences such as surgery or injuries. In most cases, secondary lymphedema is caused by the removal of lymph nodes and damage to lymph vessels during cancer therapy. For example, the lymph nodes in the surrounding area of a tumor may need to be removed as a precautionary measure to prevent the formation of metastases. This interrupts and disturbs the natural drainage of lymph fluid. Another common cause of damaged or hardened lymph vessels is cancer treatment by means of radiotherapy. If the intact part of the lymphatic system cannot compensate for the damage caused, this can sooner or later lead to lymphedema.
If lipedema remains untreated for a long time and the lymph transport is impaired, it can result in a mixed form called lipo-lymphedema.
Causes for damage to the lymphatic system:
- Surgery and/or radiation
- Injuries and bruises
- Infections caused by fungi, parasites, insect bites etc.
- Malignant diseases (e.g. tumors)
- Inflammation of the skin (e.g. erysipelas)
Symptoms – How can you diagnose Lymphedema?
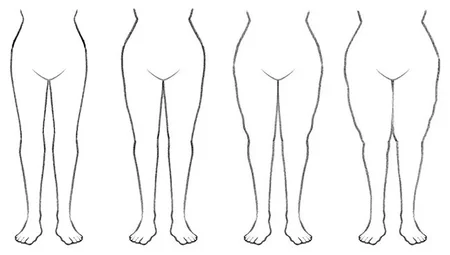
Chronic lymphedema is characterized by unilateral swelling of body parts where the tissue fluid cannot be removed properly. It usually affects the arms and legs, although lymphedema can also occur in the organs, head or genitals. Unfortunately, the available data on the number of affected people is insufficient. Estimates vary between 80,000 and 2.2 million adults who are suffering from lymphedema. However, one thing is certain: women are more frequently affected than men.
In general, a specialist can easily diagnose lymphedema by conducting a basic examination.
Depending on their severity, the following symptoms can indicate a disease of the lymphatic system:
- Extremities are unilaterally swollen, i.e. asymmetrical.
- A feeling of tension.
- It is difficult to press dents into the swollen tissue.
- The skin is slightly discolored.
- The skin is increasingly changing: it is firm and smooth.
- The skin is more prone to irritation and inflammation.
- It is difficult or impossible to lift the fold of skin over the back of the toes or fingers (positive Stemmer's sign).

Course of the disease – stages of Lymphedema
Lymphedema develops slowly and can therefore be divided into different stages of development. While lymphedema is not visible at the beginning, the swelling increases with the severity of the edema. This triggers further mechanisms that cause the lymphedema to deteriorate further without appropriate treatment.
The accumulation of protein-rich tissue fluid leads to the proliferation (fibrosis) and hardening (sclerosis) of connective tissue as well as changes in the skin, including chronic skin inflammation. These in turn support bacterial skin infections, such as erysipelas, which put additional strain on the lymphatic system and its function for the immune system. For this reason, early and continuous treatment is particularly important to prevent the disease from progressing further.
We can distinguish the following stages of Lymphedema:
Stage 0: Latent (invisible) edema
The lymphatic system is already damaged, but at this stage the affected patient is free of symptoms, since the outflow of tissue fluid can still be compensated for by the undamaged part of the lymphatic system.
Stage I: Reversible (regressive) edema
The lymphatic system is impaired and the affected body parts become swollen during the course of the day. During stage I, the tissue swelling is soft, making it possible to push in a dent. It is also possible to lift a fold of skin on the backs of the fingers or toes (negative Stemmer's sign). If the affected limbs are elevated, the swelling will go down again.
Stage II: Spontaneous irreversible edema
During stage II, excess connective tissue has already formed (fibrosis). It is no longer possible to reduce the tissue swelling by elevating the limb. The tissue is also hardened (sclerosis) and it is almost impossible to press in dents. It is no longer possible to lift a fold of skin above the back of the toe or finger (positive Stemmer's sign). In addition, the first skin changes become visible.
Stage III: Elephantiasis
The connective tissue has continued to grow and is even more hardened. The swellings take on extreme forms and there may be thickened and wart-like growths. The skin changes are also very pronounced. The skin is extremely sensitive and, as wounds heal only with difficulty, is susceptible to skin infections such as erysipelas.




